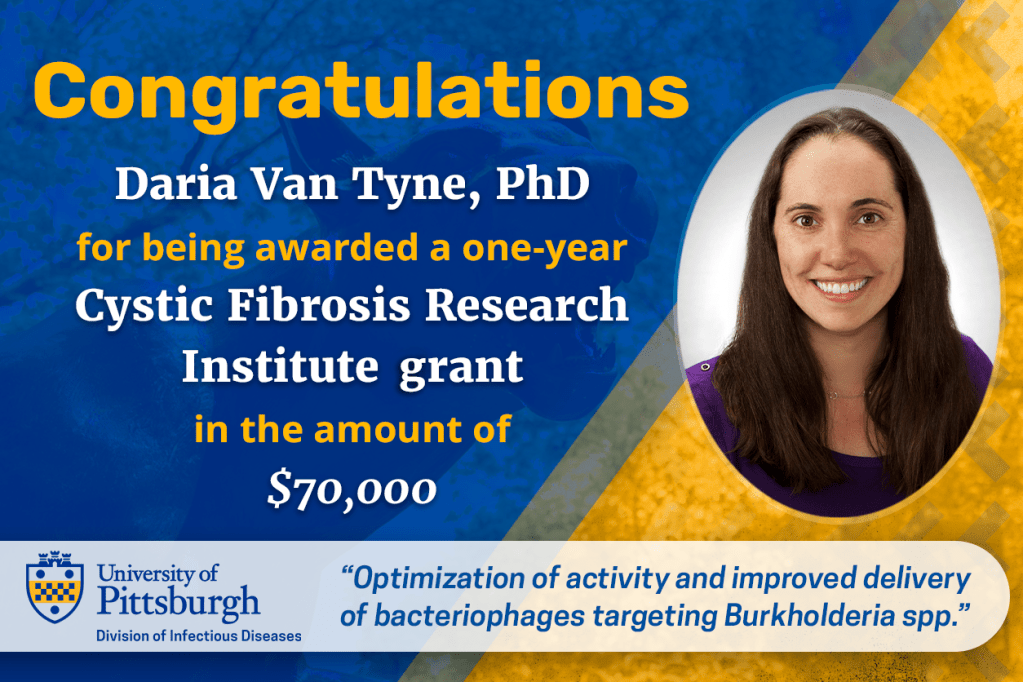
We are pleased to announce that Daria Van Tyne, PhD, has been awarded funding in the amount of $70,000 for a one-year grant by the Cystic Fibrosis Research Institute entitled, “Optimization of activity and improved delivery of bacteriophages targeting Burkholderia spp.” This proposal was submitted in response to the competitive funding opportunity entitled, “Elizabeth Nash Fellowship and New Horizons Program.”
Burkholderia cepacia complex (BCC) is a group of closely related bacterial species associated with poor clinical prognosis in patients with cystic fibrosis (pwCF). These bacteria are highly antibiotic-resistant, and some strains can cause rapid and fatal necrotizing pneumonia. Dr. Van Tyne’s team will combine their prior experience providing phage therapy to pwCF with an existing BCC clinical strain repository and phage libraries collected across three laboratories to optimize activity and improve delivery of bacteriophages targeting BCC. The Van Tyne laboratory will work with collaborators at the Center for Innovative Phage Applications and Therapeutics (IPATH) at the University of California San Diego, the Burkholderia cepacia Laboratory and Repository (BcLR) at the University of Michigan, the Center for Phage Technology (CPT) at Texas A&M University, and the Israeli Phage Therapy Center (IPTC) at Hebrew University, to conduct systematic phage susceptibility testing of approximately 40 BCC-targeting phages against 120 BCC clinical isolates collected from 60 pwCF assessing synergy of phages paired with antibiotics that are frequently used to treat BCC infections in pwCF. The goal is to identify phages and phage-antibiotic combinations that hold the most promise for treating BCC infections in pwCF.
Phages are often aerosolized for inhaled delivery, and this treatment route is frequently used for antibiotic delivery in pwCF. Ideally, phage aerosolization for inhaled therapy should preserve phage activity and should deliver phage throughout the airways. Using a previously developed computational model to determine phage doses that generate specific target concentrations in the airway will allow the team to optimize inhaled phage delivery in vitro prior to application in compassionate use protocols and clinical trials. Successful completion of this project will address critical barriers to progress in the development of phage therapy and will provide more effective BCC phage therapy to more pwCF. This study will also provide important pre-clinical information that will contribute to further development of this therapeutic modality as it moves toward clinical trials aimed at treating BCC infections in pwCF.
Please join us in congratulating Daria!


Leave a comment